Humanitarian Device
Humanitarian Device. Authorized by Federal Law for the use in the treatment of free perforations, defined as free contrast extravasation into the pericardium, in native coronary vessels or saphenous vein bypass grafts ≥ 2.75 mm in diameter. The effectiveness of this device for this use has not been demonstrated.
Indications
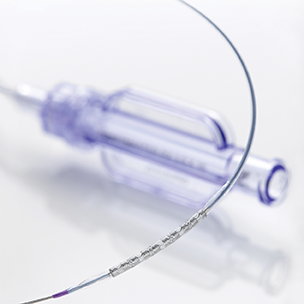
The GRAFTMASTER™ RX is indicated for use in the treatment of free perforations, defined as free contrast extravasation into the pericardium, in native coronary vessels or saphenous vein bypass grafts ≥ 2.75 mm in diameter. The effectiveness of this device for this use has not been demonstrated. Long-term outcome for this permanent implant is unknown at present.
Contraindications
GRAFTMASTER™ RX is contraindicated for use in:
- Patients in whom antiplatelet and/or anticoagulation therapy is contraindicated.
- Patients who are judged to have a treatment area that prevents complete inflation of an angioplasty balloon or proper placement of the stent graft.
Warnings
- Ensure that the sterile barrier has not been opened or damaged prior to use.
- Judicious selection of patients is necessary, since the use of this device carries the associated risk of subacute thrombosis, vascular complications, and / or bleeding events.
- Persons allergic to 316L stainless steel (including the major elements iron, chromium, nickel, molybdenum) or PTFE may suffer an allergic reaction to this implant.
- When multiple stents are required, stent materials should be of similar composition. Placing multiple stents of different metals in contact with each other may increase the potential for corrosion. The risk of in vivo corrosion does not appear to increase based on in vitro corrosion tests using an L-605 CoCr alloy stent (MULTI-LINK VISION® Coronary Stent) in combination with a 316L stainless steel alloy stent (MULTI-LINK TETRA Coronary Stent).
Precautions
General Precautions
(See also Individualization of Treatment in IFU)
- Implantation of the stent graft should be performed only by physicians who have received appropriate training.
- Subsequent restenosis may require repeat dilatation of the arterial segment containing the stent graft. The long-term outcome following repeat dilatation of endothelialized stent grafts is unknown at present.
- Care should be taken to control the guiding catheter tip during stent graft delivery, deployment, and balloon withdrawal. Before withdrawing the stent graft delivery system, visually confirm complete balloon deflation by fluoroscopy to avoid guiding catheter movement into the vessel and subsequent arterial damage.
- Carefully read all instructions prior to use. Observe all warnings and precautions noted throughout these instructions. Failure to do so may result in complications.
- Note the product “Use by” date specified on the package.
Stent Graft Handling – Precautions
- This device is intended for single-use only; do not reuse. Do not resterilize, as this can compromise the device performance and increase the risk of cross contamination due to inappropriate reprocessing.
- Do not remove the Stent Graft from its Delivery System. Removing the Stent Graft from the Delivery System may damage the Stent Graft and/or lead to Stent Graft embolization.
- The delivery system should not be used in conjunction with other stents.
- Special care must be taken not to handle or in any way disrupt the Stent Graft position on the Delivery System. This is most important during placement over the guide wire and advancement through the hemostasis valve adapter and guiding catheter hub.
- Excessive manipulation (e.g., rolling the mounted Stent Graft) may cause dislodgment of the Stent Graft from the delivery balloon.
- Do not manipulate, touch, or handle the stent graft with your fingers, as this may cause contamination or dislodgement of the stent graft from the delivery balloon.
- Use only appropriate balloon inflation media. Do not use air or any gas medium to inflate the balloon as it may cause uneven expansion and difficulty in deployment of the Stent Graft.
Stent Graft Placement – Precautions
Stent Graft Preparation - Precautions
- Do not prepare or pre-inflate balloon prior to stent graft deployment other than as directed. Use the balloon purging technique described in Section 10.2.3 of the GRAFTMASTER™ RX IFU Delivery System Preparation.
- While introducing the delivery system into the vessel, do not induce negative pressure on the delivery system. This may cause dislodgement of the stent graft from the balloon.
- Use guiding catheters which have lumen sizes that are suitable to accommodate the stent graft delivery system (See section 10.1 of the GRAFTMASTER™ RX IFU – Materials Required or product label).
Stent Graft Implantation - Precautions
- Pre-dilatations of the vessel must take into account proximal atherosclerotic plaque beyond the treatment area, which may prevent advancement of the device to the treatment area. Failure to do so may increase the difficulty of stent graft placement and cause procedural complications.
- Implanting a stent graft may lead to dissection of the vessel distal and / or proximal to the stent graft, and may cause closure of the vessel, requiring additional intervention (e.g., coronary artery bypass surgery, further dilatation, placement of additional stents, etc.).
- If more than one Stent Graft is required, the distal Stent Graft should be placed initially, followed by placement of the proximal Stent Graft. Stent Graft placement in this order obviates the need to cross the proximal Stent Graft when placing the distal Stent Graft, and reduces the chances for dislodging the proximal Stent Graft.
- Do not expand the Stent Graft if it is not properly positioned in the vessel (See Stent Graft/System Removal – Precautions)
- Placement of the Stent Graft will compromise side-branch patency.
- Do not exceed the rated burst pressure (RBP) as indicated on the product label. Monitor balloon pressures during inflation. Use of pressures higher than specified on the product label may result in a ruptured balloon with possible intimal damage and dissection.
- An unexpanded stent graft may be retracted into the guiding catheter one time only. An unexpanded stent graft should not be reintroduced into the artery once it has been pulled back into the guiding catheter. Subsequent movement in and out through the distal end of the guiding catheter should not be performed, as the stent graft may be damaged when retracting the undeployed stent graft back into the guiding catheter.
- Stent graft retrieval methods (use of additional wires, snares, and / or forceps) may result in additional trauma to the vasculature and / or the vascular access site. Complications may include bleeding, hematoma, or pseudoaneurysm.
Stent Graft/System Removal – Precautions
Removal of the delivery System Prior to Stent Graft Deployment:
- If removal of the stent graft system is required prior to deployment, ensure that the guiding catheter is coaxially positioned relative to the stent graft delivery system, and cautiously withdraw the stent graft delivery system into the guiding catheter.
- Should unusual resistance be felt at any time, either during lesion access or during removal of the Delivery System post- Stent Graft implantation, the Delivery System and guiding catheter should be removed as a single unit. This must be done under direct visualization of fluoroscopy.
Withdrawal of the Stent Graft Delivery System from the Deployed Stent Graft
- Deflate the balloon by pulling negative on the inflation device. Confirm balloon deflation under fluoroscopy and wait 10 – 15 seconds longer.
- Position the inflation device to “negative” or “neutral” pressure.
- Stabilize guide catheter position just outside coronary ostium and anchor in place. Maintain guide wire placement across the stent graft segment.
- Gently remove the stent graft delivery system with slow and steady pressure.
- Tighten the rotating hemostatic valve.
Note: If, during withdrawal of the catheter, resistance is encountered, use the following steps to improve balloon rewrap:
- Re-inflate the balloon up to nominal pressure.
- Repeat steps 1 through 5 above.
- Failure to follow these steps and / or applying excessive force to the delivery system can potentially result in loss or damage to the stent graft and / or delivery system components.
- If it is necessary to retain guide wire position for subsequent artery / treatment area access, leave the guide wire in place and remove all other system components.
- Retrieval methods (i.e., additional wires, snares, and / or forceps) may result in additional trauma to the coronary vasculature and / or the vascular access site. Complications may include, but are not limited to, bleeding, hematoma, or pseudoaneurysm.
Post-Stent Graft Placement – Precautions
- Care must be exercised when crossing a newly deployed stent graft with an intravascular ultrasound (IVUS) catheter, a coronary guide wire, a balloon catheter, or delivery system to avoid disrupting the stent graft geometry, apposition, and / or geometry.
- Antiplatelet therapy should be administered post-procedure (See Individualization of Treatment in IFU). Patients who require early discontinuation of antiplatelet therapy (e.g., secondary to active bleeding) should be monitored carefully for cardiac events. At the discretion of the patient’s treating physician, the antiplatelet therapy should be restarted as soon as possible.
- If the patient requires imaging, see MRI Statement.
MRI Statement
- Nonclinical testing has demonstrated that the GRAFTMASTER™ RX Coronary Stent Graft, in single and in overlapped configurations up to 44 mm in length, is MR Conditional. It can be scanned safely under the following conditions:
- Static magnetic field of 1.5 or 3 Tesla
- Spatial gradient field of 2500 Gauss/cm or less
- Maximum whole-body-averaged specific absorption rate (SAR) of 2.0 W/kg (normal operating mode) for up to 15 minutes of scanning for each duration of a sequence
- The GRAFTMASTER™ RX stent graft should not migrate in this MRI environment. Nonclinical testing at field strengths greater than 3 Tesla has not been performed to evaluate stent graft migration or heating. MRI at 1.5 or 3 Tesla may be performed immediately following the implantation of the GRAFTMASTER™ RX stent graft.
- Stent graft heating was derived by using the measured nonclinical, in vitro temperature rises in a GE Excite 3 Tesla scanner and in a GE 1.5 Tesla coil in combination with the local specific absorption rates (SARs) in a digitized human heart model. The maximum whole body averaged SAR was determined by validated calculation. At overlapped lengths of up to 44 mm, the GRAFTMASTER™ RX stent graft produced a nonclinical maximum local temperature rise of 1.8ºC at a maximum whole body averaged SAR of 2.0 W/kg (normal operating mode) for 15 minutes. These calculations do not take into consideration the cooling effects of blood flow.
- The effects of MRI on overlapped stent grafts greater than 44 mm in length or stent grafts with fractured struts are unknown.
- As demonstrated in nonclinical testing, the image artifact extends approximately 15 mm from the device, both inside and outside the device lumen, when scanned using the sequence: gradient echo in a 3T GE Sigma HDxt software release 15.0_M4_0910.z MR system with a Body Transmit coil. Therefore, it may be necessary to optimize the MR imaging parameters for the presence of the GRAFTMASTER™ RX stent graft.
- It is suggested that patients register the conditions under which the implant can be safely scanned with the MedicAlert Foundation (medicalert.org) or an equivalent organization.
Potential Adverse Events
Adverse events (in alphabetical order) that may be associated with the use of GRAFTMASTER™ RX Coronary Stent Graft in native coronary arteries may include:
- Acute myocardial infarction
- Arrhythmias (including ventricular fibrillation and ventricular tachycardia)
- Coronary Artery Bypass Surgery
- Death
- Dissection
- Drug reactions to antiplatelet agents/contrast medium
- Emboli, distal (air, tissue or thrombotic emboli)
- Emergent Coronary Artery Bypass Surgery
- Hemorrhage, requiring transfusion
- Hypotension / Hypertension
- Infection and pain at insertion site
- Ischemia, myocardial
- Perforation
- Pseudoaneurysm, femoral
- Restenosis of stented segment
- Spasm
- Stent graft embolization
- Stent Graft thrombosis / occlusion
- Stroke/Cerebrovascular Accidents
- Total occlusion of coronary artery