Every complex case is unique, and no calcified lesion is the same. That’s why we focus on providing the therapies, tools, and specialized knowledge that enable you to tailor your approach and optimize long-term, durable outcomes.

Our comprehensive portfolio offers individualized solutions for every step in the treatment of calcified lesions from ACCESS to CLOSE.
Gain access with the right guide wires.

Visualize the best path forward with OCT and full physiology.

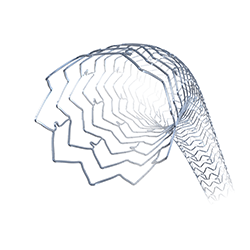
Clear obstacles with orbital atherectomy and coronary dilatation catheters.


Manage hemostasis efficiently

MAT-2408224 v2.0
You are about to enter an Abbott country- or region-specific website.
Please be aware that the website you have requested is intended for the residents of a particular country or countries, as noted on that site. As a result, the site may contain information on pharmaceuticals, medical devices and other products or uses of those products that are not approved in other countries or regions
Do you wish to continue and enter this website?
MAT-2305078 v1.0